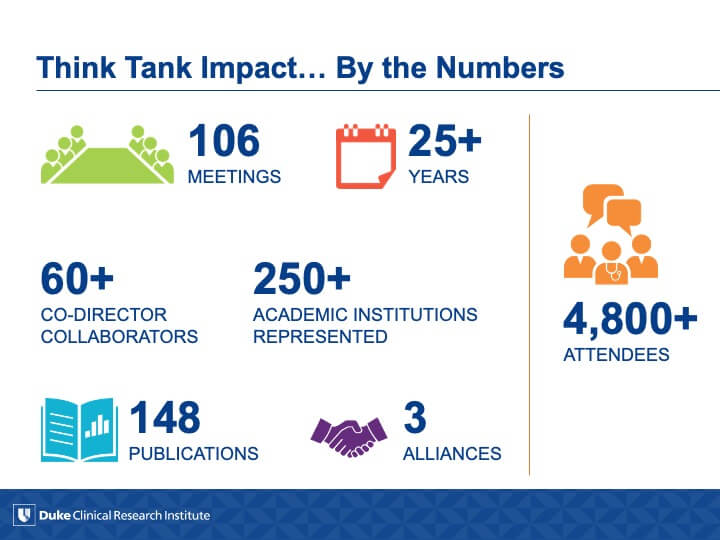
DCRI Think Tanks demonstrate what is possible when you bring smart people together to tackle the biggest challenges in clinical research. From cardiovascular diabetes to the Pediatric Rule to the Modern Data Monitoring Committee, these meetings are about creating pathways to useful, focused discussions across the healthcare continuum and then moving consensus to action.
Our mission: to address the most critical gaps in clinical research by convening leaders across the healthcare industry to map the way forward in designing, conducting, and implementing high-quality, evidence-based research.
2022 DCRI Think Tank Annual Impact Report
Although the COVID-19 pandemic posed ongoing challenges in 2021-2022, the DCRI Think Tank series continued to address critically important topics in clinical research.
With input from the Think Tank Advisory Board, we examined the durable innovations that have emerged from COVID-19, identified ways to increase access to clinical trials and improve community engagement in clinical trial “deserts”, and highlighted opportunities and challenges as more trials shift from a brick-and-mortar approach to a “click-and-mortar” approach. We also tackled the inevitability of a future pandemic and identified strategies to improve pandemic responsiveness based on lessons learned from COVID-19.
Recent DCRI Think Tanks
On January 24-25, 2024, a DCRI think tank session on “Embracing Generative Artificial Intelligence (AI) in Clinical Research and Beyond” brought together leadership from academia, industry, government, agency, and payer groups to explore the current and potential future application of AI/Large Language Models (LLMs) in clinical research, considerations for review and validation of their outputs, privacy and security concerns, regulatory considerations and needs, and ethical concerns. This meeting brief provides an overview of the key themes and actionable items from the session.

DCRI

Vanderbilt University

Duke University
Duke Fellow
On October 25-26, 2023, a DCRI Think Tank session on “Realigning Incentive Structures to Accelerate Evidence Generation” brought together leadership from academia, industry, government agencies, and nonprofit organizations to explore how different entities and influencers in drug development and healthcare can realign incentive structures to efficiently accelerate evidence generation that addresses the highest public needs. This meeting brief provides an overview of the key themes and discussions that took place during the session.
Key Takeaways and Themes
- Misalignment of incentives and priorities: Incentives and priorities in the healthcare system, allocation of resources, determination of outcome measures, and consensus on areas of highest public health needs are not currently aligned toward common goals to improve public health. The COVID-19 pandemic catalyzed a clear alignment of incentives among all stakeholders, leading to accelerated evidence generation; however, as the pandemic subsided, incentives shifted back to individualistic priorities among stakeholders. There are many challenges in defining priority areas of research with distinctions between top-down approaches that involve identifying research priorities from a centralized or authoritative perspective versus bottom-up approaches, which involve grassroots efforts and community engagement in escalating areas of greatest need. Ultimately, a consensus developed that both bottom-up and top-down approaches are valuable in determining areas of greatest need. Achieving a successful alignment of priorities among various stakeholders will necessitate changes in financial and policy incentives. These incentives can take the form of direct mechanisms like value-based care models or indirect mechanisms such as public reporting of a health system’s participation in clinical trials.
- Patient-centered approaches: The need for patient perspectives and involvement emerged as a significant theme. There was a call for greater engagement of patients in clinical research, inclusion of measures of patient experiences, and minimizing burdens imposed on clinical trial participants to improve the overall patient experience in trial participation. Patients have an important role in advancing clinical care through trial design and participation, building trust with underrepresented or disadvantaged patient populations, and grass root or bottom-up approaches to engage all stakeholders in determining areas of greatest need. Furthermore, patient advocacy groups are also key with their ability to drive policy changes and maintain long-term engagement with legislation to help define priority areas of research.
- Transparency and accountability in research: Transparency is crucial, not only in reporting results, but also for understanding allocation of funding and ensuring quality of outputs. Central to transparency is the clear communication of results to regulatory bodies and the public, with an emphasis on excluding unnecessary data that may cloud interpretation of the results. Additionally, there is a need to disseminate not only successes but also failures in order to prevent recurrent and costly errors. This approach underscores the importance of learning from past experiences of the entire clinical research community. Finally, there are opportunities to improve reporting metrics related to patients’ clinical trial experience and efficient use of resources at an institutional level to support trial enrollment and follow-up.
- Efficiency and streamlining clinical trials: There are needs to optimize recruitment and data collection, streamline study design, and efficiently leverage existing trial and care infrastructure. While technology serves a valuable role in accelerating enrollment and patient engagement in trials, careful consideration should be made so as not to inadvertently exclude underrepresented populations through over-use of technology. Streamlined trial design should be leveraged to ensure ease and accessibility for clinicians who serve as gatekeepers between patients and clinical trials and there needs to be more effective utilization of available resources, infrastructure, and technology to enhance clinical trial efficiency. Electronic health records should continue to transform to facilitate research and data collection, early cessation of the clinical development of drugs or other interventions that show early signs of failure, and identification of patient allocation to one study that may curtail opportunities for that patient to participate in other trials.
- Public-Private Partnerships: Alignment of priorities requires the need to collaborate more effectively across different industry sectors, regulatory bodies, healthcare systems, and academic organizations to accelerate the generation of evidence. Industry partners frequently embrace a risk-averse approach in anticipation of regulatory challenges to drug approval. This caution often results in adoption of rigid, standardized research protocols. Such protocols potentially burden patients and research sites by collecting unnecessary data and by relying on less efficient clinical trial procedures. Maximizing the benefits of these partnerships and streamlining research processes requires a more balanced, redistribution of risk and control. Initiating such changes entails reevaluating roles, responsibilities, and expectations of all stakeholders so as to distribute risks related to the process of regulatory drug approval process and influence of trial design more equitably.
Actionable Items
- Define research priorities and align financial incentives with impact on population health outcomes: Develop a health agenda with input from academia, industry, government, patient advocates, and payer groups to align public health priorities across stakeholders. Critical to the success of this endeavor will be to align these priorities with financial incentives that reward the impact of outputs and outcomes. A shift towards more pay for performance/ value-based care models and public reporting of performance metrics of clinical trial enrollment and health system participation in clinical trials has the potential to support these goals.
- Implement initiatives to increase patient involvement and reduce patient and clinician burden in clinical trials: Successful clinical trial design must address and alleviate patient and clinician burden in trial participation. To do so, create programs to educate patients about the importance of their roles in research design and conduct, address barriers to participation, and elicit feedback from clinical trial participants to ensure that research is designed with patients’ needs and experiences in mind.
- Enhance accountability in research participation and transparency in research progress: Develop patient- and center-specific performance metrics of research participation and success. This includes capturing information on patient recruitment numbers and diversity as well as information related to the success of clinical trials and their ability to robustly answer clinical questions. Invest in public reporting mechanisms that provide information on the quantity and quality of research outputs aimed at incentivizing high-quality clinical trials while discouraging those that fall short. Share organizational experiences, positive and negative, to promote vicarious learning and reduce resource waste.
- Redistribute risk and decision-making ability in public-private partnerships: Continue multi-stakeholder dialogue to redistribute risk allocation and influence trial design within public-private partnerships to allow for more mutually beneficial relationships for the ultimate well-being of the public.
Meeting Directors & Fellow

Sir Martin Landray, FMedSci
University of Oxford

Jeeyon Grace Rim, MD
DCRI Fellow
Format: Virtual
The FDA Commissioner recently stated that “the distortions and half-truths of misinformation and disinformation pose enormous dangers to the effectiveness of science and to public health itself, through the negative impact it has on individual behavior.”
This two-day Think Tank will delve into the critical role of key stakeholders, including the FDA, NIH, patient advocacy organizations, pharmaceutical companies, academia, and others, in addressing the dangers of misinformation and its impact on population health.
Day one will focus on challenging our concept of the misinformer, recognizing the strong motivation of social identities and affinities in information spread. We will also examine misinformation within the broader ecosystem, clarifying stakeholder roles, effective approaches, and trans-disciplinary collaborations. Day two will take a deeper dive through the lens of the clinical encounter, with attention to the “information diet” as a social determinant of health and how to best equip the next generation of clinicians to address misinformation threats. Finally, we will discuss next steps using a “whole-of-society” framework, calling on past successes in population health and lessons learned in other disciplines to identify the most promising paths forward. Join us to tackle these vital issues and pave the way to advance population health and prevent misinformation harm.
Key Questions:
1. How can we measure, track, and assess health misinformation using established and novel methods?
2. Who are the key stakeholders in addressing misinformation, and which of their strategies are most promising?
3. How can misinformation be managed at the bedside, and how can we best prepare the next generation of clinicians?
4. What does a whole-of-society approach to information look like, and what are tools, training, and collaborations are
critical to improving patient trust and preventing harm?
Meeting Directors

Emily O'Brien, PhD
DCRI

Claire Wardle, PhD
Brown University
Improvements in both the fundamental understanding of pathophysiology and diagnostic technologies have created new opportunities to develop and test novel therapies for rare diseases and now emerging for cardiovascular disease. This presents unique challenges in evidence development, as many of the strategies for evidence generation for common cardiovascular diseases (e.g, large randomized clinical trials) are difficult or impossible to implement in rare conditions.
This think tank will focus on challenges and solutions in therapeutic development for rare cardiovascular diseases taking experiences from other rare conditions. This will include the taxonomy of the rare cardiovascular disease landscape, appropriate use of diagnostics for patients screening and identification, study design and execution, appropriate endpoints for efficacy and safety, regulatory issues, implementation science for rare diseases, ethical and safety issues, and payer models and value proposition for rare diseases.
Objectives:
- Examine the landscape of rare cardiovascular diseases and available therapeutic modalities
- Discuss the challenges surrounding evidence generation in rare cardiovascular diseases from a scientific, operational, regulatory, and statistical perspective
- Discuss the value, ethical considerations, and implementation opportunities for new therapies for rare cardiovascular disease
Meeting Directors & Fellow
A Think Tank Addressing Needs and Opportunities to Generate Evidence on How to Prevent Heart Disease with Novel Therapies
Cardiovascular diseases remain the leading cause of death and disability in the United States and globally. Although inexpensive and effective therapies are widely available to prevent and treat heart disease, they are used according to guideline recommendations less than half the time. Over the last two years, for the first time in decades, there has been a decline in life expectancy in the US and other parts of the world, in large part due to cardiovascular disease. Medical innovations are advancing at a rapid pace that can prevent, and even potentially cure, disease previously thought to be life-time chronic health conditions.
For example, hypertension represents the most important risk factor for preventable death and disability in the world, and it affects more than half of the US adult population with a disproportional burden in minorities. Only about one in four patients have their hypertension well controlled, despite effective and inexpensive therapies that are underused. Yet, there has been relatively little innovation in new treatments for cardiovascular disease due to misaligned incentives to develop novel treatments. Now there are treatments being developed that are easily administered with less frequency for chronic health conditions, such as treatments targeting RNA that can be given once or twice a year and, eventually, gene editing. Even with adequate evidence generation, innovative medical products do not reach their full potential due to mistrust in science, disinformation, physician inertia, and importantly, difficulty for treatments to fit easily into patients’ daily lives contributing to non-adherence.
To address these unmet needs, advances in science could turn towards addressing common health conditions in a similar manner to what has been targeted for rare conditions with easily administered therapies or even potentially “curative” treatments. Classes of agents include vaccines, RNA targeting and gene editing therapies, as well as device therapy like renal artery denervation. Now the range of conditions with a target of prevention or “cure” include various cardiovascular risk factors such as hyperlipidemia and hypertension. These treatments offer theoretical advantages with regards to adherence and ease of use. However, due to their novelty, there are a series of questions regarding evidence generation on benefits/risks, appropriate comparators, longitudinal safety, implementation, and payment policies.
Objectives:
• Describe the unmet need for management of chronic health conditions such as hypertension and the barriers that must be overcome
• Determine the evidence generation needed to define the impact and safety of novel treatments for patients, regulators, clinicians, and payers
• Determine needs for short versus long-term efficacy and safety of novel therapies
• Consider the potential barriers and solutions for implementation into practice
Meeting Directors & Fellow
Traditional randomized controlled trials have changed the landscape of clinical medicine and provided the framework for clinical practice guidelines yet they are expensive, burdensome, and slow. Recently, the COVID-19 pandemic required
that clinical researchers pivot away from traditional studies and use newer approaches (such as point-of-care trials) to answer critical questions in a rapid manner.
Point-of-care clinical trials are designed to co-locate clinical research studies and routine, everyday clinical care delivery (whether that is in a hospital setting, office clinic, or at home). A point-of-care trial is not a type of trial design, but rather, operational approaches to conducting clinical trials that integrate clinical research and routine care delivery. These approaches may be applied to different trial methodologies, such as pragmatic or explanatory trial methodologies. They can also be applied to more seamlessly integrate with patients’ daily life, improve diversity in clinical trials, and more comprehensively ascertain patient-centered outcomes and clinical events.
This Think Tank will explore the use of point-of-care approaches in clinical trial design and the readiness of regulatory agencies and guidelines committees to embrace the evidence that they generate.
Objectives:
- Identify key obstacles and priority solutions that obstruct or enable point-of-care trial conduct to support
- regulatory decision-making
- Identify the regulatory, healthcare system and payer incentives or barriers to enable POC trials
- Explore opportunities to minimize barriers and maximize incentives
- Discuss optimal engagement of clinicians and patients in POC trials
Meeting Directors & Fellow
Chronic diseases, including heart disease, stroke, COPD, neurodegenerative diseases, and diabetes, are, besides cancer, the leading causes of death and disability globally and the main driver of the $3.8 trillion in annual health care expenditures in the U.S. each year. The drug development process has led to countless therapeutic advances in chronic diseases over the last several decades, saving and prolonging the lives of millions of people. More recently, however, a large proportion of agents brought to market are targeted therapies for cancer and rare diseases, with relatively fewer new agents introduced for other chronic conditions. Reasons for this trend may include nancial, regulatory, and feasibility barriers, as well as a less precise understanding of the biological mechanisms underlying many chronic illnesses in comparison with cancer and rare diseases. An alignment of incentives is urgently needed to ensure that the development of effective therapeutic agents keeps pace with and ideally stems the growing burden of chronic diseases world-wide.
Objectives: The over-arching objective of this Think Tank is to examine the processes of development and market deployment for new drugs to treat common chronic health conditions with a goal of accelerating development of new therapies that deliver high value to patients and health systems.
ISSUES DISCUSSED:
- What can be learned from the cancer paradigm to accelerate drug development for the 5 most common chronic conditions besides cancer (cardiovascular disease, neurodegenerative diseases, COPD, diabetes, and stroke)?
- What are the barriers and facilitators to accelerate drug development for the 5 most common chronic health conditions?
- What are the opportunities and challenges to increasing patient access to new therapies for chronic conditions?
The Emergency Use Authorization (EUA) mechanism is central to the US response to global pandemics, such as COVID-19. It allows the US Food and Drug Administration (FDA) to respond quickly to novel threats by approving a new drug, device, or diagnostic or allowing for unapproved use of an approved drug through an accelerated authorization process, when no approved alternatives exist. To obtain authorization, evidence must support that a drug or product “‘may be effective’ to prevent, diagnose, or treat serious or life-threatening diseases or conditions,” and the known or potential bene ts of the product must outweigh known or potential risks. Since the declaration of a public health emergency due to the COVID-19 pandemic by the Secretary of Health and Human Services in February 2020, 3 preventative interventions, 400 diagnostics, and 15 therapies have received EUA and of these, 3 (less than 1%) have received FDA approval.
Objectives:
- Review the experience with EUA during the COVID-19 pandemic and the proportion of requests coming from federal versus industry sponsors and the success rate
- Summarize the quality and number of clinical trials contributing to EUA for COVID-19
- Discuss the need for additional evidence or studies post-authorization and the timeline that should be expected for the provision of the additional evidence to the FDA or to advance the drug/device to approval
- Review potential incentive structures that might need to be established to conduct large trials and studies following EUA
- Discuss streamlined approaches for getting to the highest quality data the fastest, particularly for actively approved drugs
Meeting Directors & Fellow
DCRI Think Tanks Highlights
Meeting and Publication Archive
Previous DCRI Think Tank meetings with their associated publications, dating back to 1995, are archived in 5-year increments.
THE ROLE OF MACHINE LEARNING IN CLINICAL RESEARCH: TRANSFORMING THE FUTURE OF EVIDENCE GENERATION
The authors of a recent paper published in Circulation summarized the key takeaways from a February 2018 DCRI Think Tank on finding a more flexible path for diabetes drug approval. The gathering of representatives from academia, industry, regulatory agencies, and the NIH addressed guidance issued by the FDA in 2008 that glucose-lowering therapies cannot receive approval until evidence is provided that they do not increase the risk of major adverse cardiovascular events. While envisioning a new path forward, the authors balanced safety concerns, cost, evidence generation, and trial design.
ENABLING PATIENT‑REPORTED OUTCOME MEASURES IN CLINICAL TRIALS, EXEMPLIFIED BY CARDIOVASCULAR TRIALS
A “validity argument” approach takes into account that the context of each trial is different and attempts to overcome barriers historically associated with measuring and reporting patient-reported outcomes in clinical trials. Patient-reported outcome measures hold great promise for clinical trials, but more work remains to reduce challenges historically associated with integrating these measures, write the authors of a paper recently published in Health and Quality of Life Outcomes.
DRUG DEVELOPMENT IN KIDNEY DISEASE: PROCEEDINGS FROM A MULTISTAKEHOLDER CONFERENCE
A wide range of stakeholders who attended an April 2019 DCRI Think Tank helped to identify current challenges to developing treatments for chronic kidney disease, as well as make recommendations for strategies to address these challenges. Innovations that make clinical research and drug development processes more efficient could forge a path for new therapeutics to treat kidney disease, write the authors of a paper recently published in the American Journal of Kidney Diseases.
Leaders and Partners
The DCRI Think Tanks Advisory Board

Advisory board partnerships with industry leaders help the DCRI Think Tanks program address the right topics, at the right time, with the right people. Our partners provide crucial insight and connections that go beyond DCRI's clinical and operational expertise. From guidance on attendees, framing discussion topics, and contributions to resulting publications, our advisory board members are players in the lifecycle of every event.
DCRI Think Tanks Leadership
In Support of and Collaboration with:


Connect with Us
The DCRI Think Tank program welcomes suggestions and ideas for future think tank meetings.
Contact Jennifer Gloc to share your idea or to get involved, or follow us on Twitter at @DCRINews. Look for the #DCRIThinkTank hashtag.