
APRIL 15, 2024 — Faculty experts from the Duke Clinical Research Institute (DCRI) shared insights and expertise on the latest cardiology research as part of more than 100 late-breaking studies, Meet the Expert opportunities, presentations, panels, and posters at the 2024 American College of Cardiology (ACC) Scientific Sessions on April 6-8 in Atlanta.
View the full list of DCRI presentations.
DCRI kicked off the conference with AEGIS-II and EMPACT-MI presented as part of the opening late-breaking research session. The two presentations culminated in six publications in major medical journals.
Therapy Shows Promise in Delaying Hospitalizations for Heart Failure: Results from EMPACT- MI
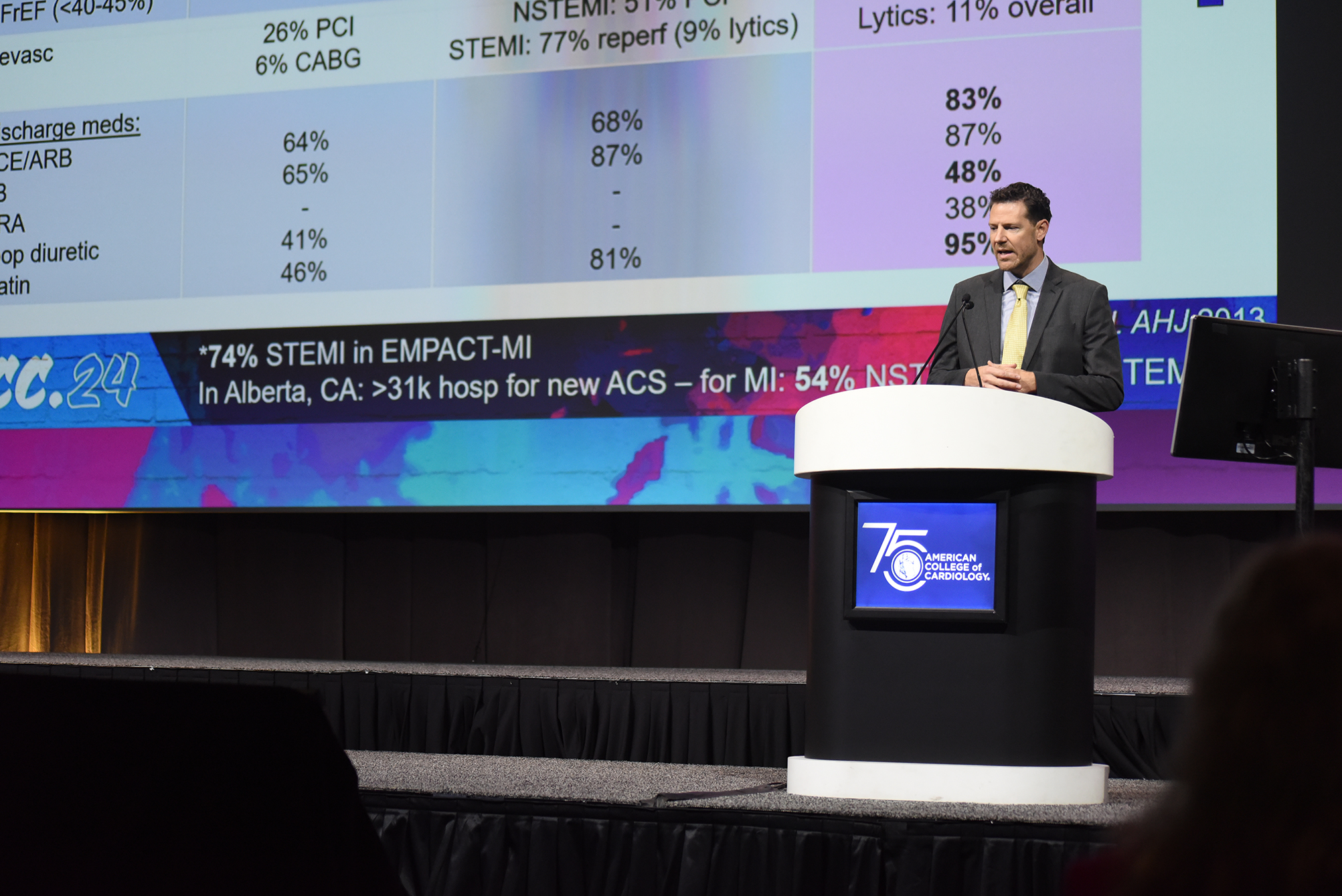
About 800,000 people in the U.S. suffer a heart attack every year, and approximately 30% of them will go on to develop heart failure. There are limited treatments to prevent or slow that development.
A large international study coordinated and conducted by the DCRI found that the diabetes drug empagliflozin (marketed under the brand name Jardiance) did not reduce deaths. Secondary findings show it did slow the time to first hospitalization for heart failure and reduced the total number of subsequent heart failure hospitalizations. The results from the EMPACT-MI trial were published simultaneously with the ACC presentation in the New England Journal of Medicine, Circulation, and the Journal of the American College of Cardiology. Details of the meta-analysis are in press in The Lancet Diabetes & Endocrinology.
The study findings on lower rates of heart failure offer some hope and underscore the importance of preventing poor outcomes after a heart attack, according to DCRI executive director and site principal investigator, Adrian Hernandez, MD, MHS.
“Developing heart failure is one of our major public health problems, and any step that gets us closer to preventing it is a step in the right direction,” Hernandez said. “After a heart attack, we should really be focused on how to prevent problems, especially the development of heart failure. This therapy fills in that gap.”
AEGIS-II Misses Primary Endpoint, but Data Suggest Further Research into HDL Modification is Warranted
Primary results from the AEGIS-II trial showed that infusions of the human plasma-derived apolipoprotein A-I CSL112 did not significantly lower the risk of major adverse cardiac events through 90 days for people who had recently suffered a heart attack. However, exploratory analysis showed that patients who received the treatment had numerically lower rates of cardiovascular (CV) death and myocardial infarction (MI), type-1 MI, and stent thrombosis-related MI compared to placebo. Primary results were published in the New England Journal of Medicine and exploratory results were published in the Journal of the American College of Cardiology.
“It’s probably the most important trial looking at HDL modification or altering HDL efficacy in terms of limiting cardiovascular events,” said DCRI’s Thomas Povsic, MD, PhD, one of the study investigators and first author of the JACC paper. “I think there are signals that it did work, but the overall effects were relatively modest and what we showed is that on certain kinds of heart attacks, it does seem to prevent downstream cardiovascular events. That would need validation in a separate clinical trial.”
Also notable from AEGIS-II was the efficiency of the study’s operations. The AEGIS-II team enrolled more than 18,000 participants across 46 countries amid the COVID-19 pandemic, with only two lost to follow-up. The DCRI managed the study data and managed the 193 U.S. sites, which enrolled more than 1,800 high-risk acute MI patients, with none lost to follow-up.
“We have long-standing relationships with many of our sites in the U.S., so I think one of the things that we bring to the table is that we know a lot of sites that will enroll well and are high quality sites that will follow their patients,” Povsic said during a Meet the Expert event following the late-breaker session. “We have relationships with country leaders throughout the world. I was one of the country leaders in the U.S., and we had a lot of contact with our sites to make sure that they were following patients and doing all the other things that we talk about in clinical trials to make sure the trial is well run, and this trial was really well run.”
DCRI’s Pagidipati Provides Practical Tips for Harnessing the Power of Anti-Obesity Medications
Anti-obesity medications squarely fit within a cardiologist’s scope of practice and should be used in combination with lifestyle changes, according to DCRI’s Neha Pagidipati, MD, MPH, presenting during a Saturday afternoon ACC session.
Referencing studies including STEP HFpEF, SELECT, STEP 1, STEP 4, SURMOUNT 1 and SURMOUNT 4, Pagidipati discussed the relevance and benefits of newer weight loss drugs such as semaglutide, liraglutide, and tirzepatide, and then outlined how she introduces patients to the medications and increases their dosing gradually.

“These patients don’t just help patients lose weight, they are CV-risk reduction agents,” said Pagidipati, underscoring the relevance of the drugs for cardiologists. She also emphasized the need for lifestyle changes in concert with the medications.
“No amount of medicine is going to help a patient become healthier if they don’t understand what they’re supposed to be doing in their life in terms of exercise and diet,” she said. “All of these studies were predicated upon some lifestyle change happening for all of these patients.”
Pagidipati went on to share the three things she discusses with her patients to ensure the medications are most effective:
- Move more: “Whatever you’re doing, do more than what you’re doing.”
- How much you eat: “It helps if you eat less, for most of us, and these agents will help us do that.”
- What you eat: “In general, I recommend the Mediterranean diet, low salt, low carb, if they’re trying to lose weight, as well.”
When starting patients on anti-obesity medications, a slow and gradually increasing approach is best.
“The key to remember is start low, go slow,” Pagidipati said. “Start at the lowest dose with patients, and I titrate every four weeks. I only titrate up to the next dose if and when their gastrointestinal symptoms have improved. If they’re queasy, have nausea, and you titrate up for them, it’s just going to get worse. Also, I tend to wait until their weight loss plateaus, and usually at four weeks it does.”
Keys to Improving Healthspan in Older Adults with Ischemic Heart Disease
During a session focused on improving healthspan in older adults with ischemic heart disease, DCRI’s Karen Alexander, MD, first sought to point out the elephant in the room: “everyone dies,” she said.
“This is not a reason that we shouldn’t be working very hard to improve quality of life before death, but we need to be aware of that, because our patients are aware of that, and as we ask them to participate in research, I think that’s on their mind to a degree.”
In aiming to generate evidence among older adults, Alexander recommended:
- considering the uniqueness of the older population, and the underlying processes unique in that age group.
- appreciating and leveraging new ways of doing research that are virtual and aligned with care.
- thinking about the outcomes that matter to the patients.
Alexander highlighted the approach taken by the ongoing PREVENTABLE study, which is finding potential participants aged 75 and older using a cohort query applied to the electronic health record. Sites then approach patients and randomize them to atorvastatin 40 mg. or placebo. Participants are tracked to determine whether they meet the primary outcome which is one that matters to the patients — survival free of dementia and persisting disability.
Researchers have made participation easy by shipping the study drug directly to patient homes and enrolling about half of the population remotely.
“This can be done,” Alexander said. “We’re having a very simple intervention, which is the atorvastatin 40 mg. versus placebo — but you could imagine how this could be replicated based on our experience in other situations.”
Keeping in mind the participant population’s desire to try new interventions is key, Alexander concluded.
“As we’re beginning to think about these fancy new interventions, we have to stop ourselves and remember the population we’re asking to go on this journey and to be in the trial boat with us. From PREVENTABLE, the one thing we have learned is that older adults are in that phase where they really don’t want to rock the boat. This is an important thing to partner with our participants and make sure they’re interested in joining us.”
What’s Now, and What’s Next for Treating High Blood Pressure?
Nearly half of adults have hypertension or are taking medication to manage hypertension. Hypertension is also known as high blood pressure, and is defined as systolic blood pressure greater than 130 mmHg or diastolic blood pressure greater than 80 mmHg.
An ACC session focused on high blood pressure reviewed the issue and the forthcoming therapies that could help to better manage the condition.
Highlighting the SPRINT study — which showed a reduction in all-cause mortality, relative risk reduction in heart failure, and reduction in stroke — DCRI faculty member Chris Granger, MD, noted that it provides a helpful example of what can be done, while also showing the limitations.
After emphasizing the study’s impressive results, Granger discussed the aftermath.

“The long-term follow-up, after two or three years after the trial was finished, the blood pressure difference between the two groups had vanished, the benefit for mortality and CV mortality had vanished,” he said. “This is in a setting where people had done the trial, they knew the benefits, it was with the same patients who knew the benefits, so this shows us that our current systems are really a failure, even in optimal settings.”
For now, key strategies for treating hypertension he highlighted include:
- targeting blood pressure less than 130 mmHg systolic for patients with or high-risk for cardiovascular disease using combination drugs titrated monthly.
- home monitoring.
- ensuring patient access to advanced practice providers, pharmacists, and algorithms measuring and promoting medication adherence.
New possibilities on the horizon could improve treatment of hypertension, Granger added.
“New treatments, like zilebesiran, I think will provide important, perhaps transformational opportunities for treating high blood pressure, in this case through a potent, what appears to be safe based on preliminary data, and sustained inhibition of the renin-angiotensin system with a treatment given once every six months as a subcutaneous injection.” he said, adding that more trials are needed and ongoing to assess efficacy and safety.
TRANSFORM-HF Modified On-Treatment Analysis Supports Primary Results
DCRI Fellow Mark Kittipibul, MD, shared results from a modified on-treatment analysis of the effects of torsemide vs. furosemide after discharge in patients hospitalized with heart failure from the TRANSFORM-HF trial.
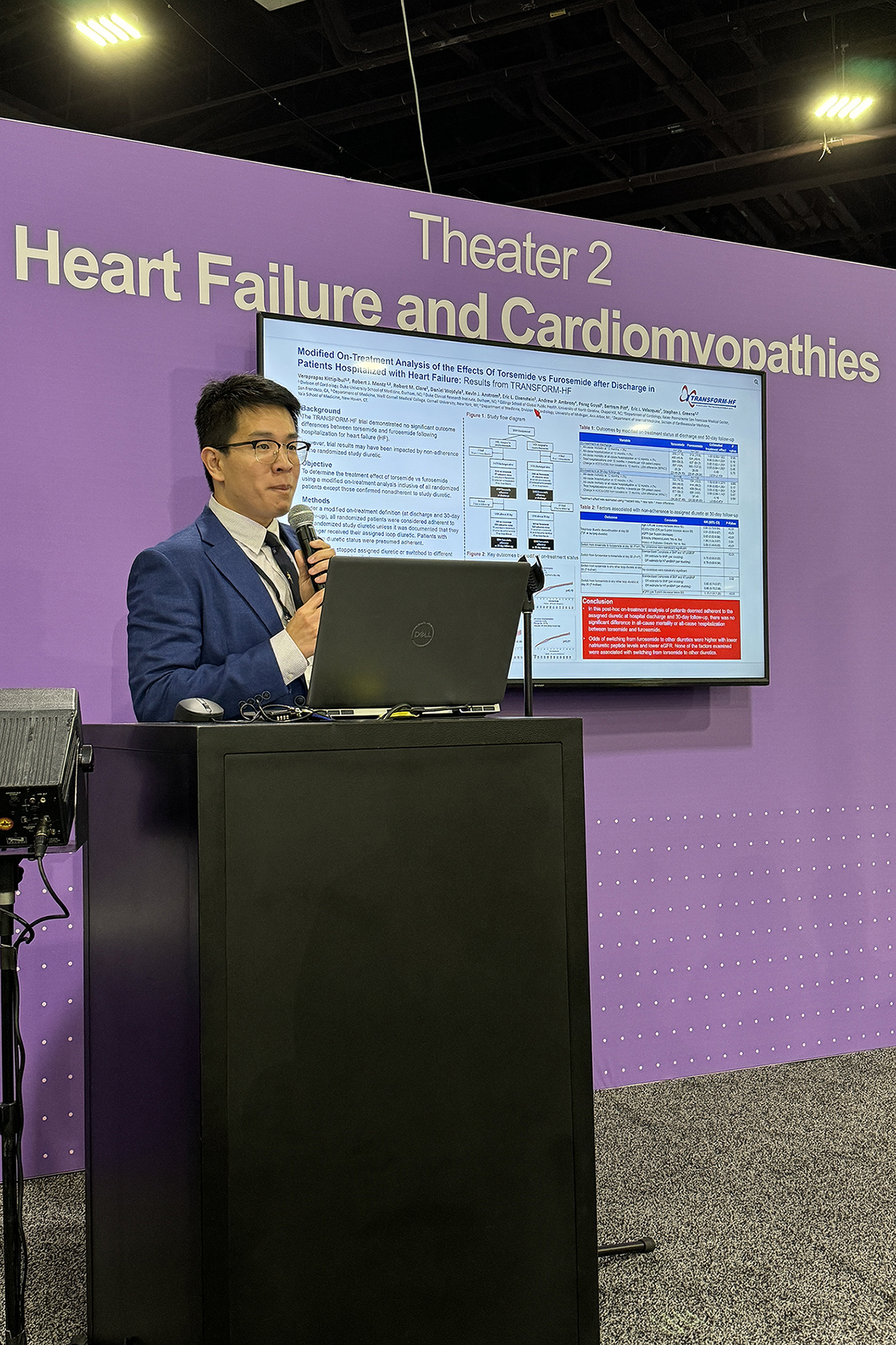
The analysis showed no significant difference in mortality between the on-treatment groups of the two diuretics at discharge or after one month.
“In this post-hoc on-treatment analysis of TRANSFORM-HF — inclusive of all randomized patients, unless they were confirmed to be non-adherent — there was no significant difference in outcomes between torsemide and furosemide,” said DCRI Fellow Mark Kittipibul at ACC reviewing the effects of the two diuretics in heart failure patients after hospital discharge. “These findings support the robustness of the primary trial results.”
Primary results from TRANSFORM-HF were first shared by DCRI’s Robert Mentz, MD, during a late-breaking science session at the 2022 American Heart Association Scientific Sessions.
New Study Shows Fortified Eggs did not Raise Cholesterol
A study led by DCRI researchers offers new evidence on fortified eggs’ health effects. In a modest-sized randomized trial, researchers found that fortified eggs — meaning those enriched with various vitamins or nutrients — did not significantly impact bad cholesterol (LDL cholesterol) or good cholesterol (HDL cholesterol) over the course of the four-month study.
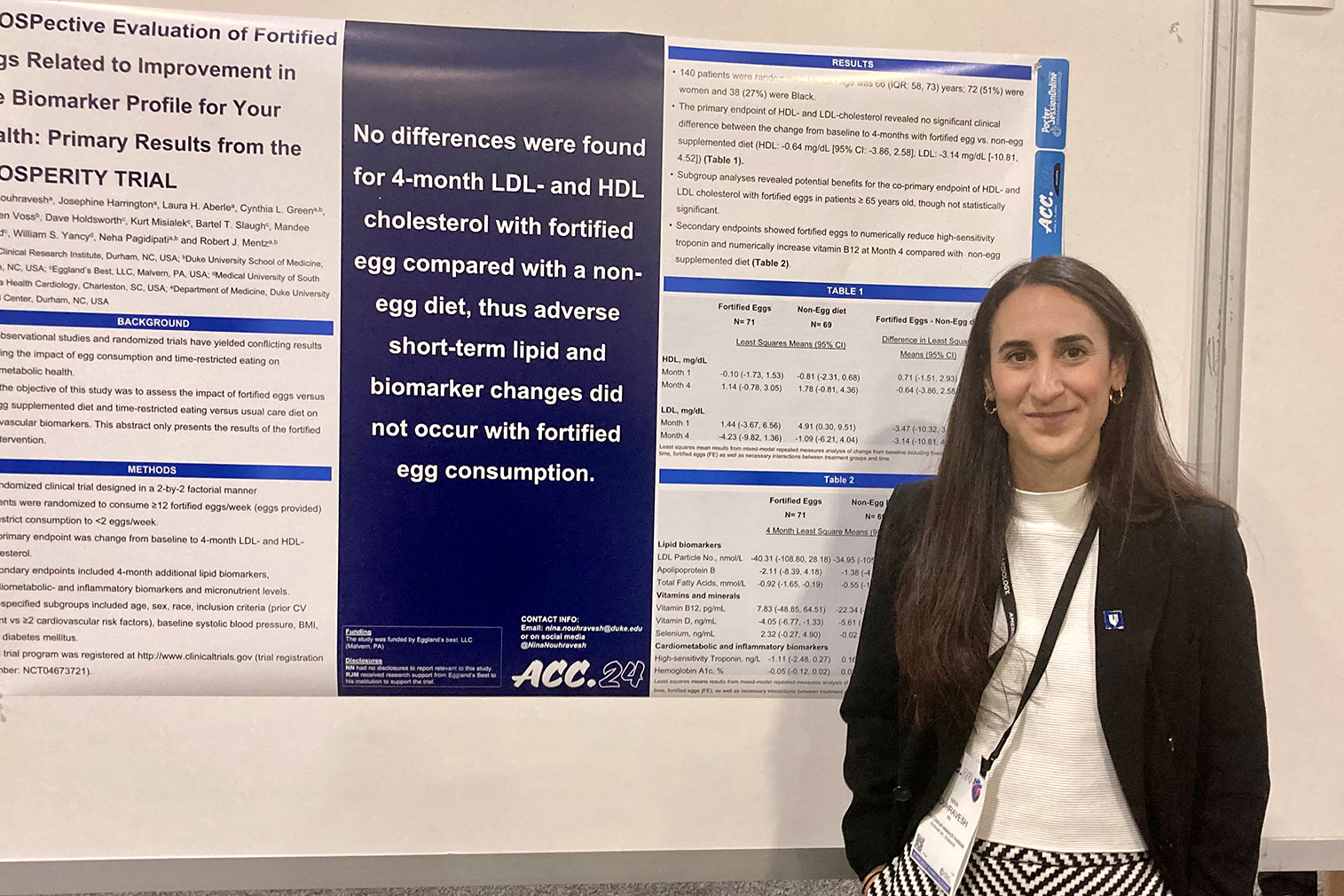
A secondary finding hinted there could be some benefit associated with fortified egg consumption for older patients and patients with diabetes. The finding was not statistically significant due to the number of study participants, but senior researcher and DCRI faculty member Robert Mentz, MD said it’s an interesting signal that the researchers would like to investigate in future work.
“While it was modest in size, it did include a broadly generalized population,” Nouhravesh said. “The average age of participants was 66 years, half were women, and more than 25% identified as Black.”
Read more about fortified eggs and cholesterol